Cancer and blood disorders are a reality that many families in Pakistan face today. Among the various treatment options, chemotherapy remains one of the most widely used and effective approaches to manage both solid tumors and haematological malignancies such as leukemia, lymphoma, and multiple myeloma. In parallel, haematology as a medical specialty plays a vital role in diagnosing, managing, and treating blood cancers and non-malignant disorders.
This article provides a comprehensive overview of oncology and haematology in Pakistan, focusing on chemotherapy, the treatment process, side effects, costs, and the importance of specialized teams and aftercare.
What is Chemotherapy in Haematology?
Chemotherapy, often referred to as “chemo”, involves the use of powerful drugs that kill or suppress rapidly dividing cells. In haematology, chemotherapy is particularly crucial for the treatment of blood cancers (haematological malignancies) such as:
- Leukaemia (AML, ALL, CML, CLL)
- Lymphoma (Hodgkin and Non-Hodgkin)
- Multiple Myeloma
- Myelodysplastic Syndromes (MDS)
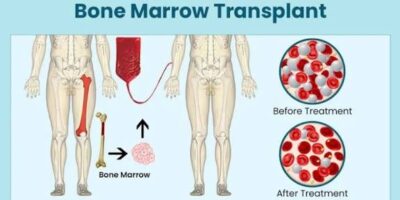
Chemo can be given alone or in combination with other therapies like immunotherapy, targeted therapy, radiotherapy, or bone marrow transplantation (BMT).
In Pakistan, chemotherapy services are available in major oncology and haematology centers, including the National Institute of Blood Disease & Bone Marrow Transplantation (NIBD), Aga Khan University Hospital, and Shaukat Khanum Memorial Cancer Hospital, ensuring accessibility for both solid tumors and haematological cancers.
Types of Chemotherapy in Oncology & Haematology
Chemotherapy is categorized based on its timing and purpose:
- Neoadjuvant Chemotherapy: Used before surgery or transplant to shrink tumors or reduce disease burden.
- Adjuvant Chemotherapy: Given after surgery or transplant to kill residual cancer cells.
- Induction Chemotherapy: Common in haematology, especially leukemia, aimed at achieving remission.
- Consolidation/Maintenance Chemotherapy: Used in blood cancers to sustain remission and prevent relapse.
- Palliative Chemotherapy: For advanced stages, aimed at symptom relief and improved quality of life.
How Chemotherapy Works in Blood Cancers
Chemotherapy drugs target rapidly dividing cancerous blood cells. However, because normal blood cells in the bone marrow also divide quickly, side effects such as low blood counts, infections, and anemia are common in haematological malignancies.
Modes of administration include:
- Intravenous (IV): Most common in oncology and haematology wards.
- Oral medications: Especially for chronic leukemias (e.g., imatinib for CML).
- Intrathecal chemotherapy: Delivered into cerebrospinal fluid for leukemia involving the CNS.
Treatment is usually cycle-based, with rest periods in between to allow recovery.
Chemotherapy & Haematology Care in Pakistan: The Process
- Diagnosis & Staging:
Blood work (CBC, bone marrow biopsy, flow cytometry, cytogenetics, molecular tests) and imaging. - Treatment Planning:
A multidisciplinary team of oncologists, haematologists, pathologists, and radiologists decides the treatment course. - Pre-Treatment Counseling:
Families are guided on side effects, lifestyle adjustments, and expected outcomes. - Administration of Chemotherapy:
Delivered in specialized day-care chemo units or during hospital admission, especially for high-dose induction regimens. - Monitoring & Supportive Care:
Continuous monitoring of blood counts, infections, and organ functions is critical in haematology. Supportive medicines (growth factors, antibiotics, antifungals, transfusions) are provided. - Post-Treatment Support:
Regular follow-up, relapse detection, psychosocial support, and in some cases preparation for stem cell or bone marrow transplant.
Common Side Effects of Chemotherapy in Haematological Malignancies
- Severe fatigue
- Hair loss
- Nausea and vomiting
- Mouth sores
- Infections due to neutropenia (low WBC count)
- Anemia and bleeding tendency due to low platelets and red cells
- Weight loss and loss of appetite
Haematology patients require extra supportive care, including blood transfusions, growth factors (like G-CSF), and infection control measures.
Cost of Chemotherapy & Haematology Treatment in Pakistan
Costs vary depending on cancer type, stage, and whether supportive haematology care is required.
- Government hospitals: Around PKR 150,000 – 200,000 for standard chemo cycles.
- Private hospitals: Ranges from PKR 400,000 – 2 million, especially if targeted therapy or transplant is needed.
- Bone Marrow Transplant (BMT): Can cost PKR 3.5 – 7 million in Pakistan.
Centers like NIBD offer financial counseling and collaborate with welfare organizations to make treatment accessible for underprivileged patients.
Choosing the Right Haematology & Oncology Center
For optimal care, select a hospital that provides:
- Experienced haematologists and oncologists
- Multidisciplinary tumor boards for personalized care
- Specialized chemo day-care units
- Bone marrow transplant (BMT) facilities
- Emergency & intensive care support
- Access to targeted therapies and clinical trials
Trusted centers in Pakistan include:
- NIBD & BMT, Karachi
- Aga Khan University Hospital, Karachi
- Shaukat Khanum Memorial Cancer Hospital, Lahore & Peshawar
- Armed Forces Bone Marrow Transplant Center, Rawalpindi
After-Treatment & Survivorship Support
Recovery for haematology patients often extends beyond chemotherapy:
- Regular follow-up tests for relapse monitoring
- Nutritionists & physiotherapists to rebuild strength
- Psychological counseling for emotional well-being
- Palliative care for advanced stages to relieve symptoms
Final Thoughts
Facing cancer or a blood disorder is overwhelming, but awareness, timely diagnosis, and access to specialized haematology and oncology care can improve survival and quality of life.
Chemotherapy in Pakistan is advancing, with better drugs, expert oncologists, haematologists, and improved supportive care to minimize side effects. While the costs may be high, financial assistance programs and welfare organizations offer hope for many families.
If you or your loved one is seeking treatment, consult a qualified haematologist or oncologist at a trusted center. Early intervention, continuous monitoring, and strong after-care are powerful tools in the fight against both solid tumors and haematological malignancies.